
The principle of the clinical EOG is demonstrated schematically in fig.1. The recorded horizontal potential difference UH is a function of the position α of the eye with respect to the electrodes and the CRP. If only eye movements between two targets are executed α is constant. The recorded potential difference UH is now only a function of CRP and indirectly of luminance. If the retinal function is disturbed the clinical EOG changes. More information from an earlier description of the clinical EOG below.
fig.1

It is a well-established fact that recordings of the corneo-retinal potential (CRP), which is largely generated by the retinal pigment epithelium, can provide an objective measure of the functional state of the retina. In the electro-oculogram (EOG) the light response of the CRP is determined indirectly by measuring its horizontal component during horizontal eye movements of constant amplitude (Arden et al., 1962). The accuracy and reliability of the results are dependent on the precise detection of the fixation periods in the eye movement recordings. DC-recordings are the basis for a precise analysis of these periods and elimination of artifacts.
fig.2

The device presented is easy to operate, so that the computer-controlled, automated procedure can be administered by a technician or nurse.This allows the professional to spend more time interpreting the data than acquiring them. Thus, this new device puts a tool into the hands of clinicians, practitioners and researchers that is much more powerful than methods used in the past. The device was built according to standards set by the International Society for Clinical Electrophysiology of Vision (Marmor and Zrenner, 1993).
In order to minimize artifacts from body motion, measurements are conducted with the patient in a reclining position looking into a spherical Ganzfeld stimulator (fig.2). Independent DC-EOG recordings of the left and right eyes are obtained simultaneously.
Stimulation: Dark adaptation is achieved by gradually reducing Ganzfeld illumination logarithmically over a range of three decades (64 to 0.064 cd . m -2). This reduces the influence of previous light stimulation and prevents the common problems of interaction between dark and light responses (Täumer et al., 1974). After 30 minutes of adaptation the program generates a sudden luminance step of four decades up to 640 cd . m-2, but other time courses can be easily programmed as required. During the procedure the patient is required to perform repeated eye movements between two alternating fixation lights (LEDs) at ± 20 deg eccentricity in the horizontal plane, while LED brightness is proportional to that of the background.
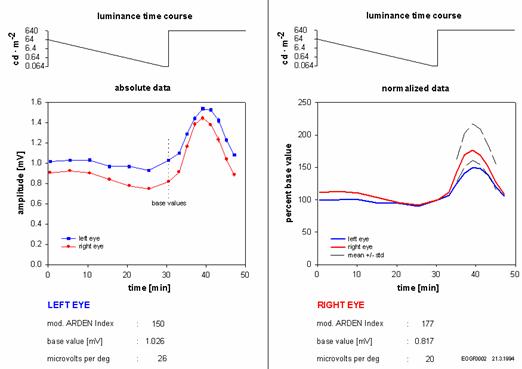
The original data of the recording can be stored on disks for later evaluation. The summarized results are printed out, along with the patient’s general profile. The data can be displayed either as absolute values (fig.3 left side) in millivolts, or in a normalized form (fig.3 right side), with the amplitude directly before the luminance step serving as reference (base value). This normalization facilitates comparison of left- and right-eye light responses. Dashed lines represent the means ± standard deviations from 15 healthy subjects. The Arden index can be calculated from the maximum EOG amplitude after the luminance step and the base value and is marked “modified” with respect to the altered dark adaptation.
fig.3
Ease of handling: Data acquisition and analysis are entirely menu-driven and require no special knowledge concerning the procedure or the computer. However, to acquaint the patient with the fixation task, LEDs can be swiched on and off by hand or the procedure simulated with patient participation as often as deemed necessary. Once the recording session has started, no further supervision of the patient is required. A certain expertise is only required in the attachment of the electrodes, so that the entire recording session can be handled by a technician or nurse.
Safety considerations: In order to ensure optimum patient safety, the EOG amplifiers are optical insulated. The device is in accordance with European guidelines for medical devices.
The variability in the response to the luminance step between 15 healthy subjects was 10%, the intra-individual variability 5% (16 measurements). The accuracy of the procedure makes the demonstration of circadian changes in the CRP possible.
This procedure has been tested clinically for more than one year on patients with various pathologies (retinitis pigmentosa, vitelliform macular dystrophy, intoxication for example). The graph in fig.3 shows normalized data from a patient with a left eye macular hole. It demonstrates the reduced light response in the left eye in comparison to healthy subjects (dashed lines).
As demonstrated by Skoog et al. (1972), the CRP can be modified by pharmacological substances like alcohol, which we have replicated in a pilot study. In this case, 0.4g of alcohol per kg body weight were administered orally and changes in CRP measured indirectly at a constant illumination of 64 cd . m-2 (fig.3). This example also supports the applicability of this device and procedure in basic neuropharmacological research.
fig.4
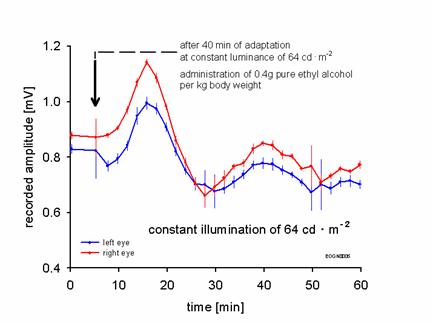
Horizontal component of CRP at constant illumination of 64 cd . m –2 after oral administration (arrow) of 0.4 g alcohol per kg body weight.
40 minutes of adaptation.
Arden G. B., Barrada A., Kelsey J. H. (1962) New clinical test of retinal function based upon the standing potential of eye. Br. J. Ophthalmol. 46, 449-467
Behrens F., Weiss L.-R. (1992) An Algorithm Separating Saccadic from Nonsaccadic Eye Movements Automatically by Use of the Acceleration Signal. Vision Res. Vol. 32,5, 889-803
Marmor F. M., Zrenner E. (1993) Standard for Clinical Electro-oculography. Arch Ophthalmol. Vol. 111, 601-604
Skoog K.-O., Textorius O., Nilsson S. E. G. (1975) Effects of ethyl alcohol on the directly recorded standing potential of the human eye. Acta Ophthalmol. 53, 710-720
Täumer R., Henning J., Pernice D. (1974) The ocular dipole – A damped oscillator stimulated by the speed of change in illumination. Vision Res. Vol. 14, 637-645
---> Back to Homepage
---> Impressum